This was a solid move. These healthcare professionals knew serving the needs of patients was paramount; with the regulatory barriers lifted, two-way video conferencing quickly met the immediate requirements to safely engage and deliver patient care.
Now, after millions of video visits executed across the U.S. by providers and staff, there is a realization of the disparity between video visits and Virtual Care. There is a difference—video visits were a quick-fix solution and now many are likely experiencing the need to pivot toward a longer-term Virtual Care strategy and technology partner.
Healthcare providers are thinking more strategically now that the first wave of COVID-19 is behind them. According to Gartner, a research firm, in its recent Virtual Care Solution report, healthcare providers are moving from initial disjointed solutions to a long-term, enterprise-wide strategy. Gartner also cautions to be mindful that the market is currently highly fragmented and there is great variation in terms of solution capabilities and cost.
“Attempting to retrofit an existing solution to a new use case may not be the cheapest, or most effective option,” say Gartner analysts in its report.1
Here are some key take-aways from our work with medical practices of all sizes:
Everybody talks about Virtual Care similarly, but they use different terms such as “video visit”, “remote care”, “telemedicine”, “telehealth”, “digital health”, and “mhealth”, among others.
Whatever you might call it, it’s here to stay and everybody wants to do it more effectively.
Medical practices all have distinct goals, processes, workflows, and organizations.
You may have ignited telehealth with video conferencing and subseqently learned that’s not working.
In one of our consults, we learned of a hospital system that was conducting 7,000+ video visits per month. They quickly learned what they needed: an efficient end-to-end solution that virtualizes every aspect of the clinical workflow from scheduling and intake, the remote visit itself, to eprescribe, discharge, and payment.
The Cost of a Fragmented Process
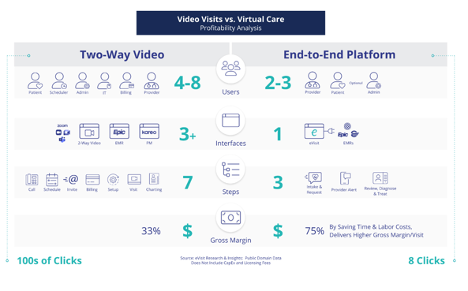
The above graphic details the significant disparity, especially the many friction points providers and staff encounter as they marry the myriad “non-virtualized” physical steps with the many team members it takes to conduct a single video visit for just one patient.
These non-virtualized steps actually take more practice staff—as many as eight people—to navigate and transact the video visit process. With video visits, there are multiple software and interfaces in play including the practice management suite; Electronic Health Record system; two-way video system, and the many team members who are phoning, emailing, texting, diagnosing, adjudicating, billing, charting, and prescribing.
Our analyses show that using an end-to-end solution saves time and labor costs and delivers a higher gross margin/visit as high as 75%.
That there is a difference between video visits and Virtual Care is one of the top lessons learned by practices during the pandemic. As you think through post-pandemic Virtual Care strategies, especially improving your capabilities to boost revenue and to serve expanding patient demand, consider this cost analysis.
15% Off Medical Practice Supplies
VIEW ALL
 Manual Prescription Pad (Large - Yellow)
Manual Prescription Pad (Large - Yellow) Manual Prescription Pad (Large - Pink)
Manual Prescription Pad (Large - Pink) Manual Prescription Pads (Bright Orange)
Manual Prescription Pads (Bright Orange) Manual Prescription Pads (Light Pink)
Manual Prescription Pads (Light Pink) Manual Prescription Pads (Light Yellow)
Manual Prescription Pads (Light Yellow) Manual Prescription Pad (Large - Blue)
Manual Prescription Pad (Large - Blue)__________________________________________________
Appointment Reminder Cards
$44.05
15% Off
$56.30
15% Off
$44.05
15% Off
$44.05
15% Off
$56.30
15% Off












No comments:
Post a Comment